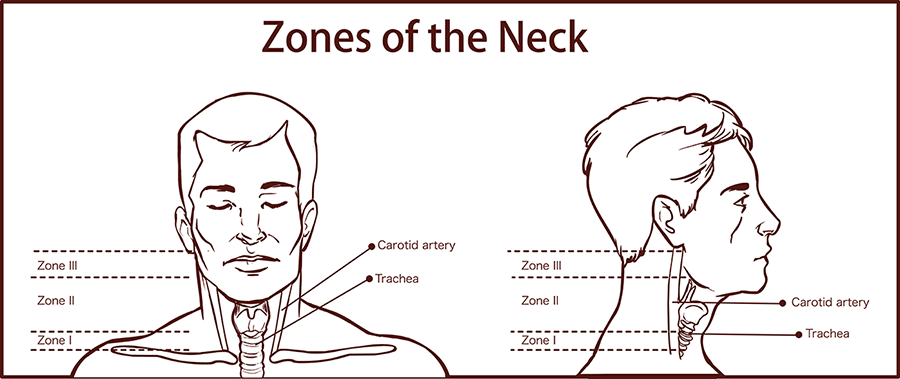
Neck trauma can cause considerable harm and pose a great challenge, as it can affect a multitude of organ systems, such as airway, vascular, neurologic, and gastrointestinal. All it takes is one single wound, for example, a neck injury that may result in the laceration of major vessels that can potentially lead to hemorrhagic shock or injury to the common carotid and vertebral arteries that can result in major neurologic deficits.The neck is divided into anatomic zones or regions to assist in the evaluation of neck injuries. The image below illustrates the zones of the neck.
What Are The Symptoms of Neck Trauma?
Symptoms vary depending on the location of the injury.
Signs of laryngeal or tracheal injury:
- Voice alteration
- Coughing up of blood or bloody sputum from the lungs or airway (hemoptysis)
- Noisy breathing (stridor)
- Drooling
- Sucking, hissing or air frothing or bubbling through the neck wound
- Subcutaneous emphysema
- Hoarseness
- Labored breathing (dyspnea)
- Distortion of the normal anatomic appearance
- Pain on palpation or with coughing or swallowing
- Pain with tongue movement
- Crepitus (crackling, crinkly, or grating feeling or sound under the skin, around the lungs, or in the joints, noteworthy in one-third of cases)
Signs of esophageal and pharyngeal injury:
- Difficulty or discomfort in swallowing (dysphagia)
- Bloody saliva
- Sucking neck wound
- Bloody nasogastric aspirate
- Pain and tenderness in the neck
- Resistance of neck with passive motion testing
- Crepitus
- Bleeding from the mouth or nasogastric tube
Signs of carotid artery injury:
- Decreased level of consciousness
- Contralateral hemiparesis (muscular weakness or partial paralysis restricted to one side of the body)
- Hemorrhage
- Hematoma
- Dyspnea secondary to compression of the trachea
- Thrill (a vibration accompanying a cardiac or vascular murmur)
- Bruit (a sound heard over an artery or vascular channel)
- Pulse deficit
Signs of jugular vein injury:
These include hematoma, external hemorrhage, and hypotension.
Signs of a spinal cord or brachial plexus injury:
- Diminished upper arm capacity
- Quadriplegia
- Pathologic reflexes
- Brown-Sequard syndrome
- Priapism and loss of the bulbocavernous reflex
- Poor rectal tone
- Urinary retention, fecal incontinence, and paralytic ileus
- Horner syndrome
- Neurogenic shock
- Deficiency in the amount of oxygen reaching the tissues (hypoxia) and hypoventilation
Signs of cranial nerve injury:
- Facial nerve (cranial nerve VII): drooping of the corner of the mouth
- Glossopharyngeal nerve (cranial nerve IX): Dysphagia (altered gag reflux)
- Vagus nerve (cranial nerve X, recurrent laryngeal): Hoarseness (altered gag reflex)
- Spinal accessory nerve (cranial nerve XI): Inability to shrug a shoulder and to laterally rotate the chin to the opposite shoulder
- Hypoglossal nerve (cranial nerve XII): Deviation of the tongue with protrusion
How Is Neck Trauma Diagnosed?
The trauma care doctor will evaluate the patient’s emergency medical reports that discuss the mechanism of injury, including the type of weapon involved, the estimated amount of blood loss (EBL) at the scene, initial vital signs, noteworthy physical findings, and total transport time.
The doctor may also order several tests to diagnose neck injuries, including:
- X-rays
- Cervical
- Chest
- Imaging Tests
- Computed tomography (CT) scanning
- Magnetic resonance imaging (MRI)
- Color flow Doppler ultrasonography
- Contrast studies of the esophagus
- Interventional angiography
- Endoscopy (used in assessing the aerodigestive tract)
- Laryngoscopy
- Bronchoscopy
- Pharyngoscopy
- Esophagoscopy
How Do You Treat Neck Traumas?
Emergency care for neck trauma begins with assessment and stabilization of the patient’s airway, breathing, and circulation (ABCs). Patients would then be transported to the closest level 1 trauma setting.
Pre-hospital care may include:
- Providing supplemental oxygen and clearing the airway of all secretions and foreign bodies, including unfastened dentures and loose teeth for the conscious patient.
- Applying impregnated gauze to cover sucking neck wounds or lacerations excluding bubbling air.
- Following cervical spine precautions for patients sustaining significant blunt trauma requiring cervical spine immobilization and supine placement of the patient on a backboard.
- Deferring removal of helmets or other headgear until neck stabilization has been ensured.
- Applying direct pressure to control bleeding from the neck.
- Delaying removal of impaled objects while in the field, and waiting to do intravenous access for removal while in route to the hospital.
- Administering prophylactic antibiotics (e.g., penicillin), if deemed necessary, to avoid infection subsequent to penetrating wounds of the neck.
- Administering massive doses of corticosteroids in selected subsets of patients to improve neurological function.
Contact Us
Go To Ortho provides full-service trauma care. We are board-certified orthopedic surgeons with privileges at all major hospitals in Portland, including some surgery centers.
Source
Walk-in appointments are welcome or you may request an appointment on our homepage or call us at 503.850.9950.



